DEFINITION
Edema is an abnormal presence of excessive fluid in the interstitial
space.
PATHOPHYSIOLOGY
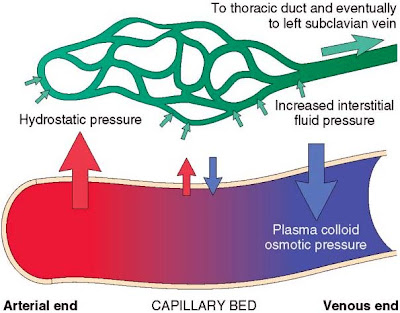
The movement of water and low molecular weight solutes
such as salts between the intravascular and interstitial spaces is controlled
primarily by the opposing effect of vascular hydrostatic pressure and plasma
colloid osmotic pressure. Normally the outflow of fluid from the arteriolar end
of the microcirculation into the interstitium is nearly balanced by inflow at
the venular end. A small residual amount of fluid may be left in the
interstitium and is drained by the lymphatic vessels, ultimately returning to
the bloodstream via the thoracic duct.
Either increased capillary pressure, diminished colloid
osmotic pressure or inadequate lymphatic drainage can result in an abnormally increased
interstitial fluid i.e. edema. An abnormal increase in interstitial fluid
within tissues is called edema, while fluid collections in the different body
cavities are variously designated hydrothorax (pleural cavity),
hydropericardium (pericardial cavity) and hydroperitoneum (the last is more
commonly called ascites). Anasarca is a severe and generalized edema with
widespread subcutaneous tissue swelling.
The diagram above shows the actual change in pressure
gradients at the capillary level. The numbers represent the pressure in the
vessels in mmHg.
At the arteriolar end, the hydrostatic pressure (outward
force) is 37 mmHg while the oncotic pressure and interstitial pressure (inward
forces) are 25 and 1 mmHg respectively. Thus the net outward force is 37 – (25+1)
= +11 mmHg. Since the net outward force is positive fluid moves from the
capillary to the interstitial spaces.
At the venular end, the hydrostatic pressure is lower and
has a value of 17 mmHg. The oncotic and interstitial pressure on the other hand
remain the same i.e. a total of 26 mmHg (25+1). Thus the net outward force is
17 – (25+1) = -9 mmHg. Since the outward force is negative, it means fluid is
not getting out of the capillary but instead it is moving into it.
The arrows in the diagram show the magnitude and
direction of net fluid movement.
CLASSIFICATION
1) According to pathophysiological mechanism:
a)
Transudate (low protein content)
b)
Exudate (high protein content)
2) According to location:
a) Localized
b) Generalized
3) According to clinical finding:
a)
Pitting
b)
Non-pitting.
LOCALIZED EDEMA
It means that the edema is localized to a specific region
of the body. It is commonly due to venous/lymphatic causes, allergy and
inflammation.
1) Venous edema: It is due to high venous pressure or
venous constriction. Intravascular venous obstruction e.g. Deep vein thrombosis
(DVT) or an external compression like a mass (tumour) or plaster are the common
causes but there can also be failure of venous pumps due to paralysis of
muscles (Cerebro-vascular accident), immobilization of parts of the body
(Post-op, fractures) and failure of venous valves (Varicose veins). It is more
frequent to see localized edema in the lower limbs but the upper limbs may also
be affected.
2) Lymphatic edema: It is due to a blockage in the
lymphatic return. It commonly occurs in conditions like cancer/ post-radiation,
infections like elephantiasis (Filaria nematodes), surgery or congenital
absence or abnormality of lymphatic vessels. The edema is persistent and
non-pitting type. In case of elephantiasis, the affected limb may be
dramatically enlarged.
3) Allergy/Angioedema (Quincke edema): During a case of
allergy there is release of histamine and other mediators that lead to
vasodilation. The swelling can involve the face, lips, tongue and even glottis.
Edema of the glottis is a medical emergency as it can lead to asphyxia if not
treated quickly. This type of edema is usually itchy but transitory. It
resolves with antihistaminics and steroids.
4) Inflammation: Here also there is vasodilation because of
the inflammatory mediators. Edema is seen with superficial (cellulitis) or deep
infections (abscess).
GENERALIZED EDEMA
In this case the edema involves more than 1 part of the
body simultaneously. It is commonly due to cardiac, hepatic, renal or endocrine
causes.
1) Cardiac edema: The initial pathology is because of
increased venous pressure but as the condition becomes more severe, there is
impairment of renal blood supply, activation of rennin-angiotensin-aldosterone
system and finally hypoalbuminemia secondary to liver stasis. Left sided heart
failure leads to pulmonary edema while right sided heart failure causes peripheral
edema, ascites, hydrothorax and anasarca in severe and long standing cases. The
edema is progressive. In ambulant individuals, it moves up with severity. The
edema is usually of pitting type. In early stages of heart failure, there is
improved renal circulation at night leading to nycturia. Thus the edema will be
less in the morning and progressively increases towards the end of the day.
2) Hepatic edema: Liver pathology like cirrhosis leads to
decreased synthesis of proteins. The hypoalbuminemia leads to decreased oncotic
pressure. The scarred liver also causes a back pressure in the portal vein
territory (portal vein hypertension) and increases the hydrostatic pressure
there. These 2 factors combined lead to edema in the peritoneal cavity (ascites)
and this in turn compresses the inferior vena cava and leads to edema in the
lower limbs.
3) Renal edema: Kidney diseases like nephritic syndrome
with decreased glomerular filtration rate and sodium/water retention or nephrotic
syndrome where there is albumin loss in the urine lead to generalized edema.
The edema frequently occurs in lax connective tissue like the face, periorbital
area and genitalia. It is of pitting type. It occurs mostly during the morning
and is associated with vasoconstriction. Thus it is called as ‘white’ edema.
4) Endocrine edema: Many endocrine problems can cause
edema. In case of hyperaldosteronism (primary or secondary), there is retention
of sodium and water. This leads to an increase in hydrostatic pressure. The
edema is of pitting type. On the other hand, myxedema refers to a non-pitting
type of edema seen in hypothyroidism. Finally, females experience edema as part
of the pre menstrual syndrome due to hormonal changes.
CAUSES OF EDEMA (ACCORDING TO PATHOPHYSIOLOGY)
- Increased capillary pressure (increased
hydrostatic pressure)
- Excessive kidney retention of
salt and water
- Acute or chronic kidney failure
- Mineralocorticoid excess
- High venous pressure and venous
constriction
- Impaired heart functioning (Congestive
heart failure, constrictive pericarditis)
- Venous obstruction (Deep vein
thrombosis, External compression like a mass or plaster)
- Failure of venous pumps
- (a) Paralysis of muscles (Cerebro-vascular
accident)
- (b) Immobilization of parts of
the body (Post-op, fractures)
- (c) Failure of venous valves (Varicose
veins)
- Decreased arteriolar resistance
- Excessive body heat
- Insufficiency of sympathetic
nervous system
- Drugs (vasodilators, calcium
channel blockers)
- Decreased plasma proteins
- Loss of proteins in urine (Nephrotic
syndrome) or G.I.T (Protein-losing gastroenteropathy)
- Loss of protein from denuded
skin areas
- Burns
- Wounds
- Failure to produce proteins
- Liver disease (Cirrhosis)
- Serious protein or caloric
malnutrition
- Increased capillary permeability
- Immune reactions that cause
release of histamine and other immune products (Allergy)
- Toxins
- Bacterial infections (Cellulitis)
- Vitamin deficiency, especially
vitamin C
- Prolonged ischemia
- Burns
- Blockage of lymph return
- Cancer
- Infections (Filaria nematodes)
- Surgery
- Congenital absence or
abnormality of lymphatic vessels
- Post-radiation.
CLINICAL FEATURES
In dependent edema, which is typically present in
congestive heart failure and in conditions associated with a low plasma protein
level, the swelling first appears at the ankles and over the dorsum of the foot
and only gradually involves the legs, thighs and trunk. The best place to check
for slight degrees of edema in an ambulant patient is behind the malleoli at
the ankles. In bed-bound patients edema often appears first over the sacrum. To
recognize pitting edema it is important to press firmly and for a sustained
period of 20-30s over a bony prominence (tibia, lateral malleoli or sacrum) to
provide effective compression. The 'pit' will be as easily felt as seen. If the
finger pressure is not maintained for an adequate period of time then slight
degrees of edema may be overlooked.
Edema can be recognized by the pallid and glossy
appearance of the skin over the swollen part, by its doughy feel and by the
fact that it pits on finger pressure.
The edema of lymphatic obstruction does not pit on
pressure or there may be minimal pitting. The skin is usually thickened and
tough.
N.B
1) Without redness and scaling, bilateral periorbital edema may indicate acute nephritis, nephrosis or trichinosis. If there is irritation, contact dermatitis is the probable diagnosis.
1) Without redness and scaling, bilateral periorbital edema may indicate acute nephritis, nephrosis or trichinosis. If there is irritation, contact dermatitis is the probable diagnosis.
2) In local venous obstruction the edema is confined to the
parts from which the return of blood is impeded. Local edema is sometimes seen
over inflamed joints.
3) Edema of the whole upper part of the body may result from
intrathoracic tumours.
Last reviewed on: 1 September 2015
Last reviewed on: 1 September 2015

Very well explained. Thank you.
ReplyDeletevery nice thank you
ReplyDeleteException... Excellent!!!!! Wonderfully explained...
ReplyDeleteAn ascent in possibly one outcomes in an ascent inside the extraordinary. This outcomes in extra of the essential. check out
ReplyDeleteThere are several resources that promise you better health and you will be able to have this kind of health.
ReplyDeleteHealth Topics